The debate around euthanasia is generally driven by ethical arguments and desperate pearl clutching. Without a doubt I feel the appeal of both arguments, life is good and there is something uncanny about providing easy and available suicide for millions of people in the name of harm avoidance. That being said, if I will ever get Alzheimer’s, I will kill myself while I am still me, legality be damned.
So, I believe that the true deciding factor when it comes to the euthanasia debate are practical matters like economics and simple arithmetic. Once the numbers favour either of the two positions it is easy to find moral justifications for mathematical calculations, but more of that later.
Definitions…
First, we have to define what euthanasia is, since it can mean quite a few things in different contexts. The most basic definiton is that euthanasia is to intentionally die (or be killed) in order to avoid unnecessary suffering. It can be passive, where one lets a terminal disease kill the patient while ameliorating the suffering or it can be active where one directly ends the life of a patient, this specific essay will be more concerned with active euthanasia.
The second important distinction is that of voluntary and involuntary euthanasia, involuntary euthanasia is not actively practiced in any country today, but the most famous historical case is the German Aktion T4. Today many countries and states have legalized voluntary euthanasia (aka assisted suicide) such as in Belgium, Switzerland, Canada and some US states such as Oregon.1
Although the euthanasia debate has been going on since the dawn of modern medicine in the 17th and 18th centuries, the actual legalization of voluntary euthanasia is exclusively a 21st century phenomenon. The first country to do so was the Netherlands in 20022, since then, it has been legalized in several other countries and the debate has resurfaced. Here is the current prevalence by country:
The Practical logic of Euthanasia
The simple fact is that at all times there are limited medical resources in any given society and these have to be allocated in one way or another, and in the cases where there is not enough for everyone, attention will be given to some and not to others according to their age, social status, and medical condition. It is precisely in these contexts when the question of euthanasia becomes relevant.
It is a fact that the people that require the largest amount of medical attention are the elderly and this means that healthcare is an industry that circles around the needs of the old. Of course, this does not mean that young people do not need medical attention, but the medical resources that the average 20-year-old receives are orders of magnitude less than the average 80-year-old.
The best-case scenario (BCS) for healthcare would be a country which is economically well-off and has a young population; there are many young people who require little medical attention (and are able to provide it), and few old people who require much of it (and cannot provide it themselves). In this case, there are enough medical resources for everyone’s needs, and thus there is no need to make the difficult choice of who gets treated and who gets left out in the cold.
But now let’s imagine the worst possible scenario (WCS); a country in severe economic hardship with a population where the old outnumber the young. In such a case, the medical resources would be strained to begin with because of the economic situation, and this would be further compounded by having millions of old people who demand constant medical attention.
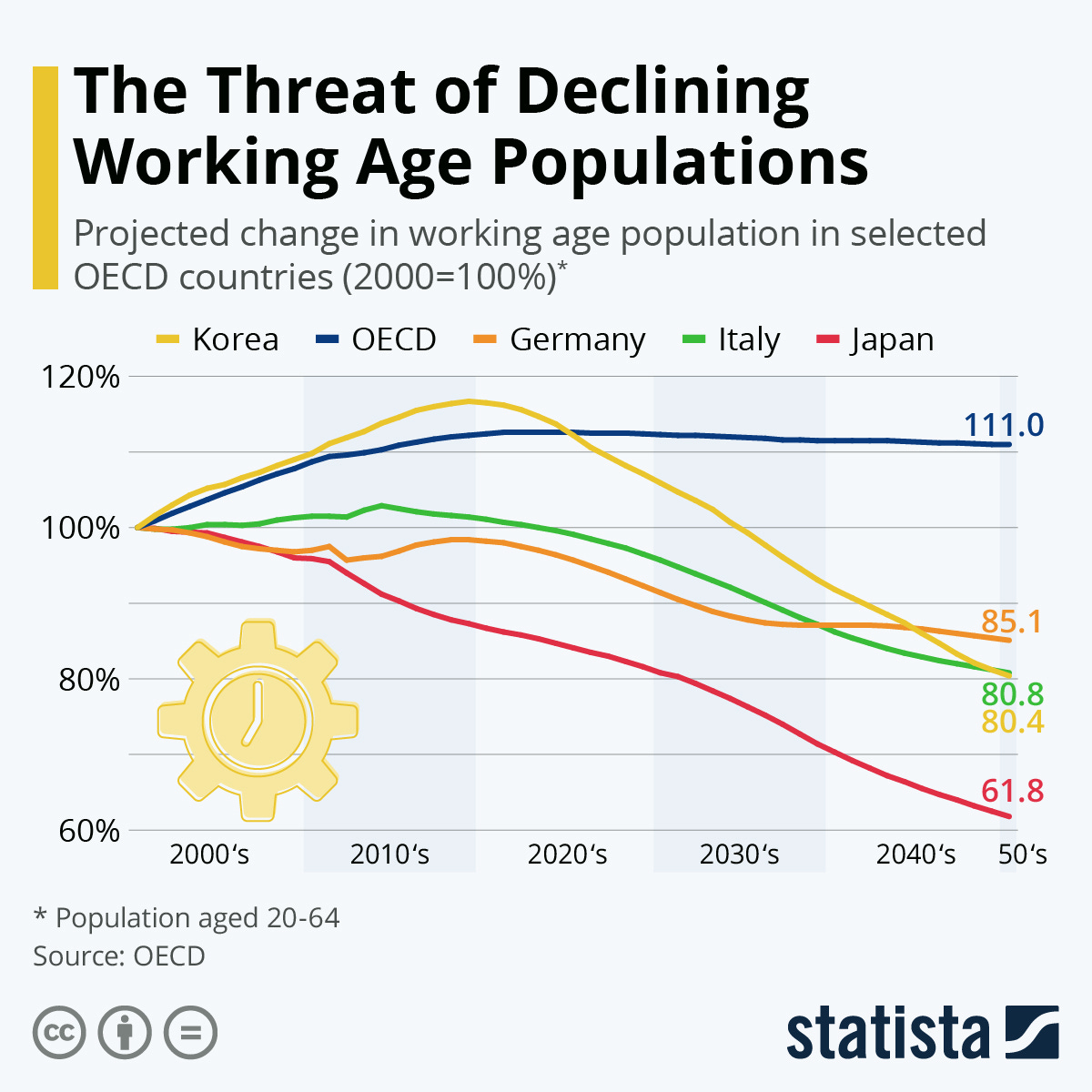
This increased demand for healthcare would fall on the shoulders of the younger generations who will have to staff the hospitals and pay (directly or indirectly) for the increased expenses of the old. But the young could not easily take over the jobs of the previous generation due to their age cohort being much smaller than that of the retirees3, the result would be evident; desperate demand and insufficient manpower which would lead to crippling prices and to many not being able to access treatment.
The question of euthanasia in the BCS is plainly ridiculous, why should one let grandma die when there are the resources available to try everything to save her? In such cases, it is easy to listen to the anti-euthanasia arguments that attempt to save lives at all costs, after all, who does not want to have all the healthcare system at their disposal when facing a deadly disease?
On the other hand, the usefulness of euthanasia becomes evident when there is an acute shortage of healthcare resources. By the nature of the practice itself, all medical professionals are in constant contact with death, indeed, the choice to treat one patient over another is fundamentally a choice over life and death. If the death of some is a given, if we cannot treat everybody, then the logical thing, the humane thing to do is to ease the suffering of the doomed through short and painless death, as opposed to prolonged agony.
Thus, it is no surprise that Canada, arguably the country with the most strained healthcare system with an average waiting time of 30 weeks to see a specialist4, is also the country most known for its euthanasia program. So far, medical assistance in dying, commonly known as MAID, has ended the lives of 60,000 Canadians.
A country like Canada is nowhere close to the worst-case scenario where the healthcare system collapses. Canadia’s economy is still strong despite its recent stagnation and although it has had a historically mediocre TFR, its population pyramid is not abysmal due to increased immigration.5
However, the point here is not to give an exhaustive report of the state of healthcare around the world, but to prove a point. Today euthanasia is a niche topic because the healthcare system of most countries is still in good shape and therefore euthanasia is not really a practical necessity.
What is indisputable is that this is changing…
Virtually all countries6 are in a process of aging, of having more old people than young people, this means that almost every single country will be very slowly moving away from the best-case scenario and sliding closer and closer to the worst-case scenario, a gradual process, but there is no way to escape the numbers.
The simple reality is that a country with more elderly people will have a higher medical demand, and a country with fewer young people will have a limited number of medical resources. Perhaps this problem will be solved by technological developments, but it does not seem to me that we are living in an age of revolutionary medical breakthroughs like penicillin, but of gradual improvements on existing technologies.
This is still no crisis and this essay is not about chanting that “the end is nigh!”, but instead, that as the demographic structure of most countries around the world shifts dramatically, the strain on their respective medical resources will also increase and that this will lead to the expansion of euthanasia programs around the world, indeed that the recent legislation in Western Europe, the US, and Australia is no coincidence.
Public v. Private?
But so far, I have been negligent. I have talked about the whole world as if their healthcare systems were run on the same model. Clearly the social consequences of a strained public healthcare system are very different to those of a private one, both show their deficiencies in very different ways.
A universal healthcare system under strain will show its problems in an increasing number of inefficiencies and shortages. Since a public system has a limited budget that cannot expand rapidly, it will simply not be able to keep up with the demand and this will lead to increased wait times and to lower service quality. The Canadian system and the British NHS are common examples of rising inefficiency.
I believe that in these systems age will be a defining factor. The people who make up the bulk of the workforce are in their 30s to their 50s while the population that most require healthcare are those about to retire or already in retirement (see above). The result is that there is a disconnect between the people who need healthcare and those who pay for healthcare and this results in conflicting interests. The workforce will want to pay less taxes for services that they do not currently require, while the elderly will want better health care since for them it's a matter of life and death.
For the moment this tension has not reached a boiling point, however one can easily observe that Western countries are spending a larger and larger share of their GDP on healthcare and that the workforce is becoming smaller and smaller as more people retire. These two trends will lead to a smaller number of taxpayers holding a larger tax burden and thus to possible political and social tensions.
One can, of course, not predict how this could play out, however, different interests do tend to reflect themselves in elections, and as the healthcare problems become crises in many countries, one could expect different parties running on programs appealing to either elderly voters or to younger ones. So, I think that it is a pretty safe prediction to say that generational tensions will get progressively worse as the century rolls on and it is possible that universal health care might be one of the catalysts.
In the countries with a privatized system the result would essentially be the same but with more steps; increased demand would raise both insurance and medical costs, this is not even speculation, it already is a tangible reality in many countries, especially in the US. However, it is also important not to treat the US as a completely privatized system since government programs such as Medicare and Medicaid represent 45% of healthcare spending with an estimated price tag of 1.5 trillion USD per year, that being said, most people (66%) have private healthcare insurance from their job.
The US also has many factors that have pushed up healthcare demand beyond just general aging. America is the major nation with the highest obesity rate in the world, America is facing a drug epidemic of historic proportions and they spend 17% percent of their GDP on healthcare, more than any other nation.
That being said, the simple fact is that in the US much like in the rest of the world, the demand for health care is outpacing the supply. The reality is that even in a market economy such as the US, there are also limited medical resources, there are limited numbers of doctors, nurses and hospital beds. It does not matter if the government, the insurance companies, or the average person is the one that ends up paying, the reality is that the system is becoming strained and many people will not receive or will not be able to afford the healthcare services they need.
This is an issue heavily tinged by social class; there are people who can afford medical treatment, those who would go bankrupt if their insurance denies their claim, those who are helped by government programs, although this often is not enough, and those who are not insured at all. There are millions of people, especially young ones, that despise the current system perhaps the figure that best embodies this tension is Luigi Mangione, indeed it is a registered fact that a large percentage7 of young people admire Luigi.
As the healthcare system becomes more strained in the foreseeable future, we can expect America to become more polarized and matters of class. It would also be a pretty safe bet to say that figures similar to Bernie Sanders are going to occupy a larger part in the discourse of the American left. However, the future of the American healthcare system is far less certain than in other countries due to the different demographic structure of its society and its own unique healthcare challenges.
The age of Euthanasia
Now that we have talked about the different possible problems that each system might face in the future, I think it is important to go back to the topic at hand which is the future of euthanasia.
The core argument of this essay is that there is a direct correlation between this strain that a healthcare system faces and its acceptance and implementation of euthanasia purely on practical grounds. The idea is that the closer that the healthcare system gets to the worst-case scenario, the more euthanasia will become institutionalized and practiced on a large scale.
If we take into account that the future prospects of both private and public healthcare systems are becoming increasingly grim, then it logically follows that euthanasia will play an increasingly large role around the world. As of today, euthanasia is not widely practiced; there have only been a handful of countries that have legalized voluntary assisted suicide and, in these countries, it remains the exception and not the rule.
However, I will argue that this is because most healthcare systems of industrialized countries are nowhere near the worst-case scenario. There are certainly systems that are facing delays and difficulties and others where medical care is becoming increasingly unaffordable, but it could be much, much worse.
Let’s make a scale where the best-case scenario stands at 1.0 and the worst-case scenario is located at 0.0. When a society is close to a score of 1, active euthanasia is unthinkable and passive euthanasia is only practiced in a handful of terminal cases. When a healthcare system finds itself around the middle of the scale, where it is under strain, but is not yet in crisis, we can expect that voluntary assisted suicide will be legalized and practiced at a small scale, much like Canada today.
If a system approaches 0, meaning that there is an economic crisis, insufficient resources, and where the choice to save one patient and let another die becomes an everyday occurrence, millions of people will prefer a quick and painless death to a long and uncertain treatment, that is if treatment is available at all.
In times of crisis, it could also be possible that euthanasia could start being involuntary in many cases. I think it is a pretty good historical rule of thumb that in desperate situations a cold and inhumane logic takes hold of a society. Simply put, if a country is in crisis and it believes that its number of elderly people is dragging the nation down with them, a very cruel sort of logic could come to fruition…
This all might seem very dramatic and unrealistic. Millions of people voluntarily committing suicide? Millions more being forced to do so? Hospitals having to decide who gets treatment and who does not on a daily basis?
This might be a valid point, however, I remain convinced that radical euthanasia programs will become a possibility if there is a sufficient crisis inside a country in which the economy, the civil society and the healthcare system cannot keep up with the needs of the population.
I'm not a doctor and much less a hospital administrator, so I'm not the indicated person to give accurate predictions of the future of most healthcare systems around the world. All that I can do is to point at the graphs and state the possible implications of a future healthcare crisis.
It is important to underline the word possible because no such health care crisis has ever existed in modern history, precisely because increased levels of aging and decreasing fertility rates are also a completely new and unprecedented phenomenon. There exists a very real possibility that within our lifetimes we will see the first country ever where the elderly outnumber the working age population. Such a drastic change will also have drastic social and medical consequences; my money is on euthanasia.
All that being said, this essay is very speculative and perhaps it will look very stupid in a couple of decades, however, I very much enjoy this type of speculation. I think that what is indisputable is that healthcare will be one of the leading political issues of the 21st century and that its social and cultural impact will be felt by all of us and probably not for the best…
The legality of passive euthanasia is a bit of a gray area, de jure, most countries hold all types of euthanasia to be illegal, but passive euthanasia is de facto legal in most coultries because it is not criminalized.
It is arguable that the swiss were the first to permit it, under the 1942 penal code suicide was only illegal in the case that it was “selfish“ and there is no direct law that makes assisted suicide legal, although if it already is de facto. Also notice the graph where the swiss assisted sucide rate was zero beginning in 1998.
This problem of having too few young people taking over the jobs of those doctors and nurses that have retired can be solved through specialized immigration, but this is at best a stopgap solution that does not address the acute lack of new professionals being formed.
https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2024
Might be a curse or a blessing for their healthcare system, results not yet in.
The only exceptions are a handful of African countries, overall interesting map.
https://ourworldindata.org/grapher/median-age?tab=map&time=2023









God stays in heaven because he's scared of his creation...
Spreadsheet brain is gay and should be punishable by forced labor in the fucking bauxite mines.